Obesity in the United States has not always been at the levels we see currently. Whenever I return from an international flight, even at the airport I sense that I have returned to the land of the big. And nowhere is this more glaring than with our children.
Beginning in approximately the mid-1980s, the levels of obesity and excess weight in the US has been a monotonically increasing function.
These averages, however, hide regional and socio-economic differences: for some sub-populations this is a medical crisis. One of 7 low-income, preschool-aged children is obese, but the obesity epidemic may be stabilizing at this alarming level. Low-income two to four year-olds’ obesity prevalence increased from 12.4 % in 1998 to 14.5 % in 2003 but rose to only 14.6 percent in 2008.
Unplanned development, migrations patterns, and sprawl have made large swaths of residential America places that discourage accidental exercise and the physical movements of everyday life, modern worklife and computer games lead to a sedentary lifestyle, and early taste training with more meals purchased outside the home than prepared load up calories, saturated fats and sodium. In Obesity, Business and Public Policy, Acs and Lyles developed the concept of an infrastructure of obesity – a reinforcing constellation of individual and societal, public and private sector factors.1
First lady Michelle Obama has made the elimination of childhood obesity in one generation her personal goal. Through the Let’sMove initiative she is focusing on the multiple factors that influence the achievement and maintenance of a healthy weight in the absence of a lifetime of dieting. It addresses Healthy Choices, Healthier Schools, Physical Activity, and Access to Affordable Healthy Foods. The Life Cycle Health Model integrates research findings into a compelling explanation of the lead time between exposures earlier in life and consequences subsequently, both for risk exposures and for preventive activities. Much current research and debate focus instead on too narrow a time spectrum for cause and effect.
What will deconstruct this infrastructure, the scaffolding on which the current obesity crisis rests?
US Constitutional Federalism reserves health authority for the states, despite evolving approaches to federalism over our nation’s history. What options are available?
Develop consensus and align independent authorities by shared goals and transparent reporting
Since 1979 the US Surgeon General has issued decennial reports on the health of the nation, the latest being HealthyPeople 2010. Of the approximately 300 goals grouped into 28 focus areas, 10 are identified as Leading Health Indicators, which “were selected on the basis of their ability to motivate action, the availability of data to measure progress, and their importance as public health issues.”: the first two are Physical Activity and Overweight and Obesity. If focusing attention were sufficient, the national obesity problem would have been solved; however, it is not. Despite the continuing focus on reducing the proportion of adults and children who are overweight and obese, all of the tracking data going the wrong direction. For example, HP Objective 19-3c. ‘Reduce the proportion of children and adolescents who are overweight or obese’ was 11% at the 1988-1994 baseline, the 2010 target was 5%, but in 2006 it was 17%. HP Objective 19-2. ‘Reduce the proportion of adults who are obese’ was 23% at the 1988-1994 baseline, had a 2010 target of 15%, but in 2006 = 33%!
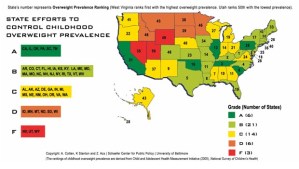
Develop a state wide legislative report card for moral suasion
Much of the development concerns children because their environments are both more controlled and more controllable in terms of exposure to fruits, vegetables, snacks, soda and junk food. Dr. Ann Cotten and colleagues at the Schaefer Center for Public Policy (SCPP) developed a report card of legislative efforts to improve the nutritional environment for children. The scores were disappointing, but the media attention did motivate some state legislatures.
Childhood Obesity Report Card 2006 (University of Baltimore)
Encourage health care providers to confront this challenge
In 2005-2006 thirty-four percent (34%) of adults in the US had a Body-Mass Index (BMI) ≥ 30 (i.e., were obese) but only 42% of obese persons were advised by a healthcare professional to lose weight.
Resolution
“Reversing obesity is not going to be done successfully with individual effort. We did not get to this situation over the past three decades because of any change in our genetics or any change in our food preferences. We got to this stage of the epidemic because of a change in our environment and only a change in our environment again will allow us to get back to a healthier place.” – Dr. Thomas R. Frieden, director of the US Centers for Disease Control and Prevention (CDC), quoted in a DHHS Healthfinder news article.
“Reversing this epidemic requires a multifaceted and coordinated approach that uses policy and environmental change to transform communities into places that support and promote healthy lifestyle choices for all people.” – As William H. Dietz, MD, PhD, director of CDC’s Division of Nutrition, Physical Activity and Obesity, quoted in a CDC press release.
The enormity of the challenge was recently emphasized when Arizona announced that it would eliminate that state’s Children Health Insurance Program for children in poverty. We have faced such challenges before and prevailed. With determination and commitment, there is every reason to believe that we will eventually do so again.

I've always thought that obesity was a result of food portions getting bigger and access to fast food getting larger. I'm glad this issue is coming to the forefront of the nations issues. The solution all starts with education and implementation.